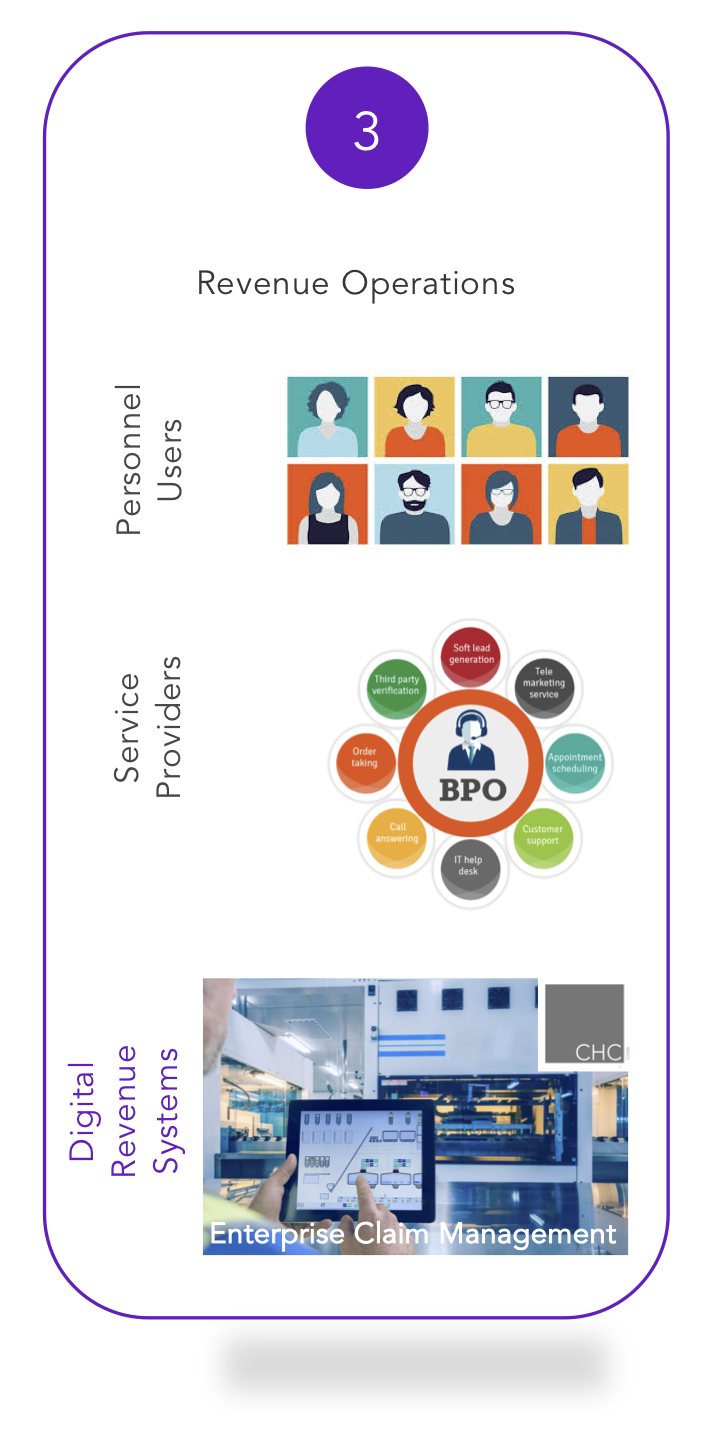
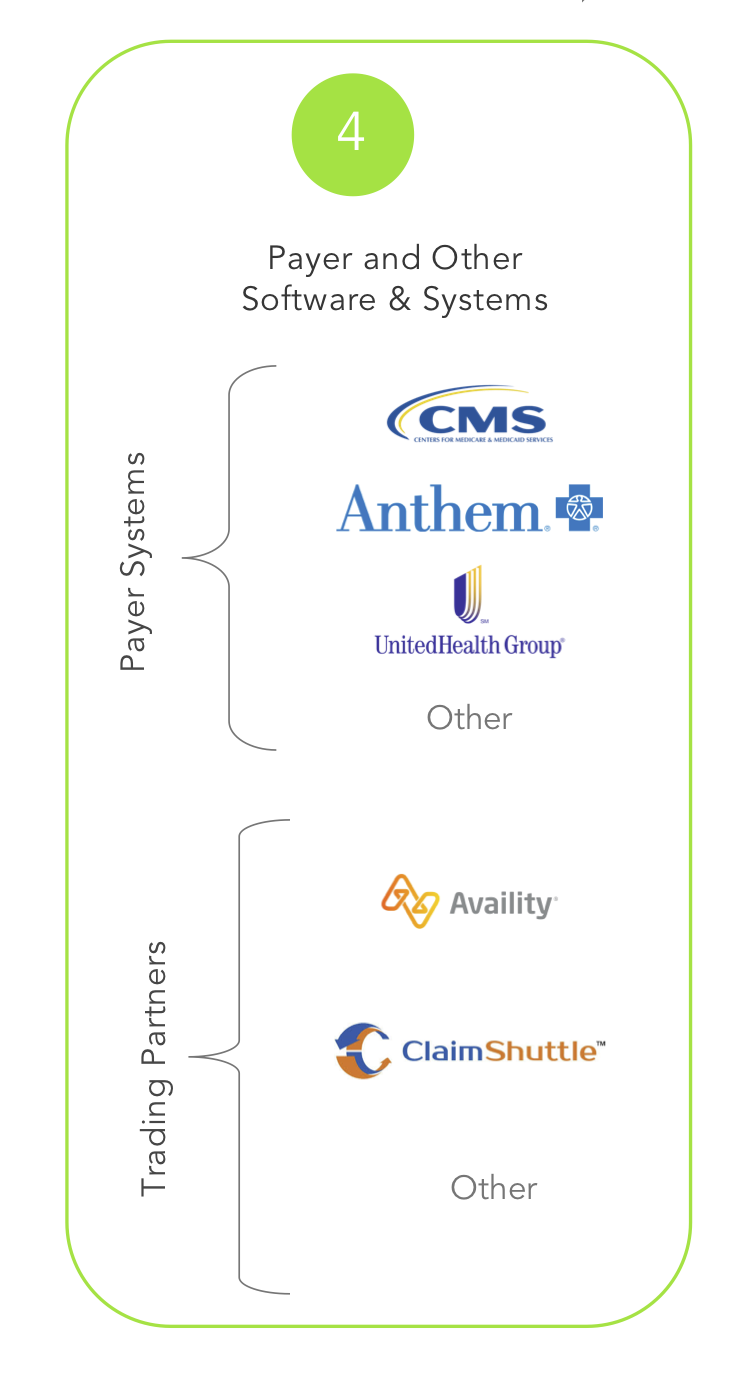
4. Payer and Other Software & Systems – Where Remittances & Denials Happen
This area is perhaps where our global view can be best described as it relates to revenue operations. Most, if not all, revenue operations consider collections as an indicator of how well they have done. Of course, the aggregate of remittances, denials, and open accounts represent collections. The largely missed but obvious fact is the most accurate data regarding collections isn’t from the providers’ systems, but rather the payers’ systems.
ECM design provides connectivity and interoperability to:
- 460* Payers including every Medicare carrier from American Sonoma to Puerto Rico and every U.S. state in between for electronic claim status inquiries. ECM connects to every payer that offers electronic claim status.
- 10,174* Payers for professional claims
- 9,776* Payers for facility claims
- 137* Payers for dental claims
This allows ECM to work with the most current and accurate data available directly from the payers’ systems – real data that matters when it comes to remittances and denials.
* As of September 2020. Subject to change. Payer enrollment and contract may be required.