Skip to content
Issues for Both Physician Groups & Hospitals
- Insurance companies, including Medicare & Medicaid, create detailed data barriers to reduce or reject claims
- Defects can be as high as 33%
- Some estimates show rejections, denials, underpayments, etc. at 15% or higher
- Many billing corrections are never made or made too late
- Too labor-intensive
- Late filing denials
- Accounts are written off to contractual (No analysis of what problems exist and are reoccurring)
What ECM Does
- ECM works as a virtual AR team member leveraging artificial intelligence to massively improve user productivity. In turn, user productivity gains translate to lower data error, timely follow-up, and higher operating margins.
- ECM identifies errors (defects) in billing, classifies them, and initiates follow-up until the final settlement of each claim line item. Data defects of up to 33% are common with current systems and processes.
- ECM improves collections (yields)
- ECM lowers the cost of managing and scaling Revenue Operations
- ECM makes a monthly financial contribution towards revenue optimization starting the second month of deployment
The ECM Difference
“For the first time, ECM makes it economically feasible to not only follow-up all high-value claims, but all claims and line items regardless of dollar value.”
-
- Unlike new employees, ECM doesn’t require any training and gets to work on day one.
- ECM works autonomously – 24×7, eliminating the need for supervision or allocating work, which saves supervisory and management time.
- ECM scales without limit as it is built as a web-scale cloud service. This allows providers to scale Revenue Operations on-demand to meet growth.
- For the first time, ECM makes it economically feasible to not only follow-up all high-value claims, but all claims and line items regardless of dollar value.
- ECM allows for machine to machine (M2M) workflows – in addition to the traditional machine to users. In having ECM – a machine, work directly with payers’ adjudication systems – other machines, human error, and limitations are eliminated. ECM frees up users to focus on tasks that have higher returns when user knowledge and experience are applied. Last but not least, M2M workflows mean ECM has the most current data for claims and defects reported directly from payer systems. Ultimately, data in payer systems are what matters when it comes to settlement of claims and getting reimbursed as expected.
- Without limits in storing and recalling every data element, ECM tracks every line item from the transmission of a claim to the final settlement.
- ECM leverages AI – specifically, machine learning to continuously learn and improve. A simple example of how ECM learns are patterns subscribers ID issued by various insurers (health plans). Every time a subscriber ID passes through one of ECM processes, ECM makes a note of the Insurer and the pattern of the subscriber ID. With every snapshot, ECM learns and develops an understanding of the patterns used by various insurers to issue subscriber IDs for their members. This knowledge is then used in identifying and flagging potential defects (subscriber Ids) that don’t meet the expected pattern.
- When ECM learns something new, the knowledge developed is codified and applied universally to the benefit of all ECM users as opposed to sitting inside the heads of a few users.
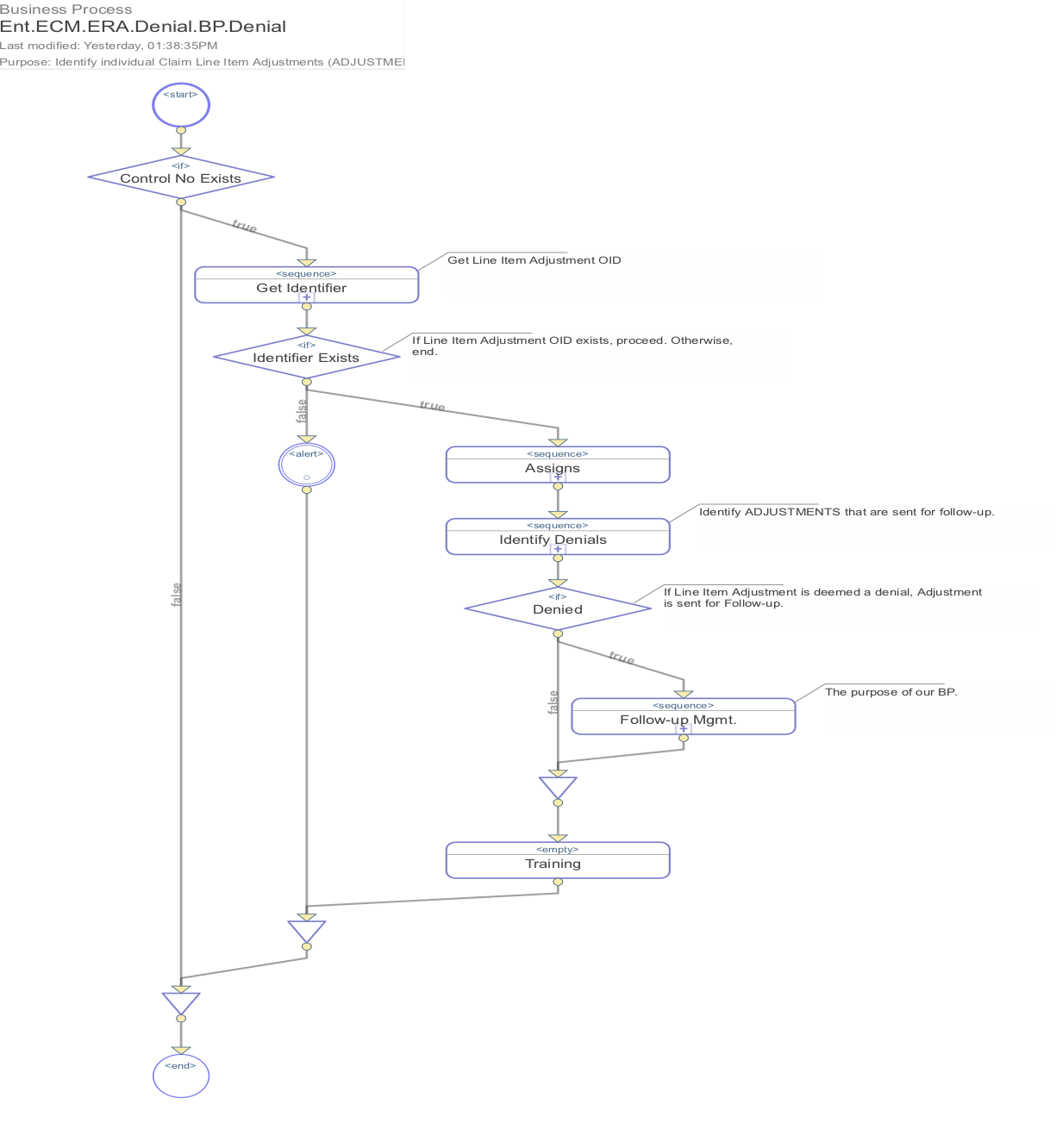
How ECM Works
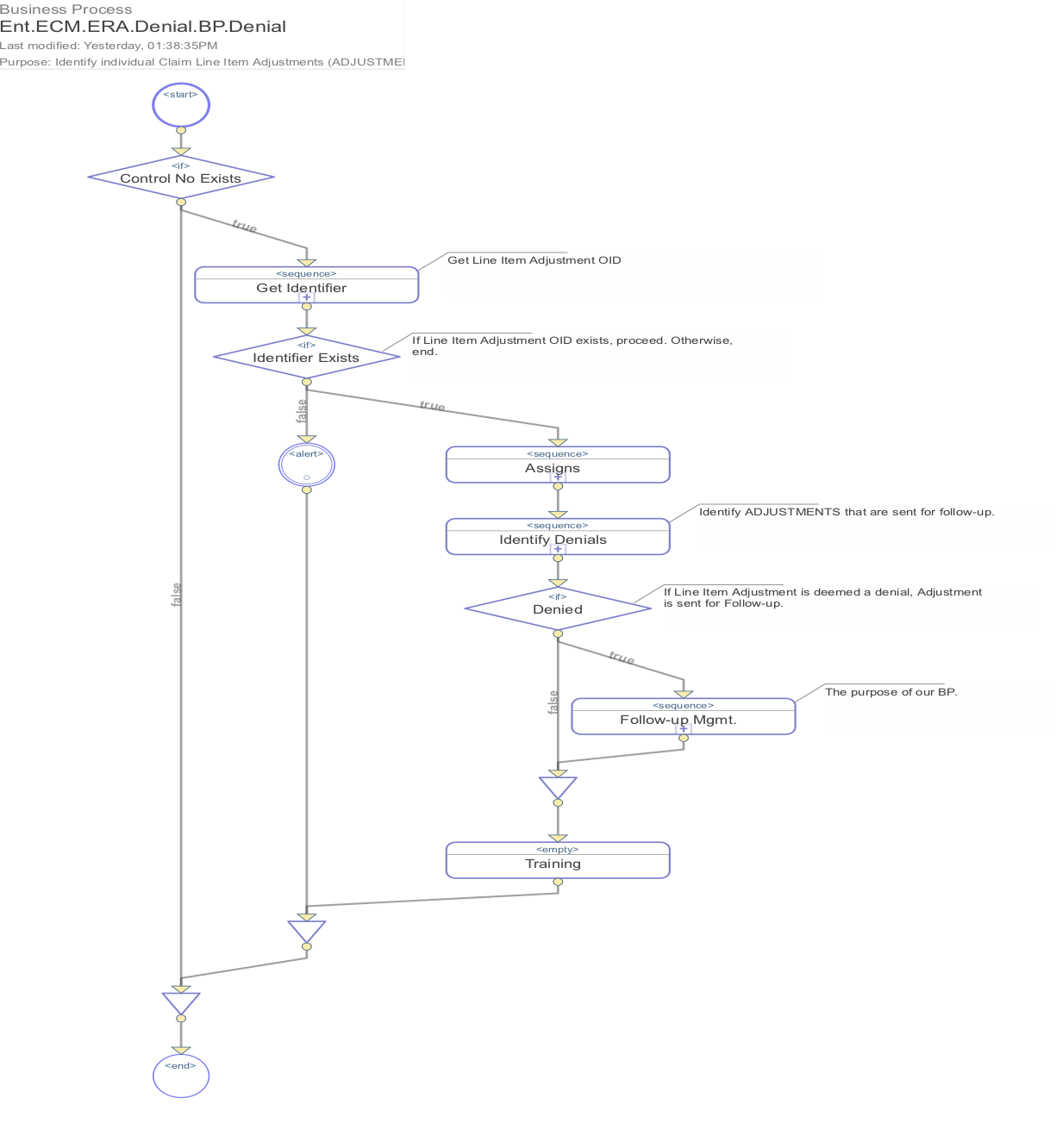
- ECM works with industry-standard EDI 835 and 837 files – AKA Electronic Remittance Advice (ERA) and Electronic claim submission. In other words, ECM works with any & all billing systems.
- In only requiring EDI files that are already generated by legacy billing systems, ECM requires no migration or integration. This allows for deployment of ECM within 30-days – including user training and onboarding.
- Using incoming EDI 835 (ERA) files;
- ECM reviews each line item adjustment to identify, classify, and route all non-contractual adjustments to user workstations for follow-up.
- ECM identifies inaccurate or updated subscriber data that may result in denial and routes claims with defective subscriber data to user workstations for correction & follow-up.
- ECM identifies inaccurate or updated payer data that will result in denial and routes claims with defective payer data to user workstations for correction & follow-up.
- ECM identifies claims transferred by payers which originally received the submission to ensure transfers were appropriate and to the correct payer.
- Using a copy of EDI 837 (claim) files sent to payers from legacy billing systems, ECM schedules at least three claim status inquiries, and based on payer response to each of the inquiries, schedules additional follow-up actions to ensure appropriate final settlement.
- 1st Inquiry – Within 3-5 days, ECM generates claim status inquiry (CSI) Requests and connects with the respective payers’ adjudication systems to ensure that all claims and line items have been received and logged into the payers’ systems as expected. For each CSI Request sent, ECM expects to receive a CSI Response. ECM uses CSI Responses to determine the appropriate follow-up actions.
- 2nd Inquiry – If initial CSI Responses are received indicating expected progress, ECM follows-up within 9-13 days with a second CSI Request regarding adjudication determination by each payer’s system. As in the first CSI Request and Response, ECM makes a determination at the line item level for appropriate follow-up actions based on CSI Responses it receives. If CSI Responses indicate defects that may result in non-contractual denial(s), ECM immediately initiates corrective actions.
- 3rd Inquiry – If second CSI Responses are received indicting expected progress, ECM again follows-up within 21-23 days with a third CSI Request regarding adjudication remittance issuance by each payer’s system to determine the status of expected remittances. Otherwise, as with the initial CSI Responses indicated defects, ECM immediately initiates corrective actions.
- ECM monitors all user workstations and escalates work items that have not been completed in a timely manner.
- ECM provides real-time reporting and analysis defects identified and improvements gained.
- ECM provides real-time reporting and analysis on its own productivity and performance. Allowing for real-time RoI calculations.
“As all providers are constrained by how much can be added to the payroll, the only alternative is to meaningfully improve the productivity of current personnel in order to improve collections. ECM makes that possible.“
ECM Results
- A Decrease or Elimination of Defects
- Improved Cash Flow
- Increased Revenue
- Decreased Expenses
- A Platform Scaled for Growth